A heart attack and heart block are two distinct cardiac conditions with different causes and manifestations. Here’s a brief explanation of each:
- Heart attack (Myocardial Infarction): A heart attack, medically known as myocardial infarction (MI), occurs when there is a blockage in one or more of the coronary arteries, which supply oxygenated blood to the heart muscle. This blockage usually results from the buildup of cholesterol plaque that ruptures and forms a blood clot, obstructing the artery. The lack of blood flow and oxygen to a section of the heart muscle can lead to damage or death of the affected tissue. Symptoms of a heart attack often include intense chest pain or discomfort, shortness of breath, pain radiating to the left arm, jaw, or back, nausea, sweating, and lightheadedness. Prompt medical attention is essential for the diagnosis and management of a heart attack, as it is a medical emergency.
- Heart block: Heart block, also referred to as atrioventricular block, is a condition that affects the electrical conduction system of the heart. It occurs when the electrical signals that regulate the heartbeat are delayed or blocked as they travel from the atria (upper chambers) to the ventricles (lower chambers). This disruption in the electrical pathway can result in an abnormally slow heart rate, which can cause symptoms such as dizziness, fatigue, fainting, or even cardiac arrest in severe cases. Heart block can have various causes, including age-related degeneration, heart disease, congenital defects, medication side effects, or electrolyte imbalances. Treatment for heart block depends on the severity and symptoms and may involve the use of medications, pacemakers, or other interventions to regulate the heart rate and restore proper conduction.
It’s important to note that while heart attack and heart block are distinct conditions, they can coexist in some cases. For instance, a heart attack may lead to damage in the conduction system, resulting in heart block as a secondary complication. Therefore, it is crucial to seek immediate medical attention if you experience symptoms suggestive of a heart attack or any concerning cardiac symptoms to receive an accurate diagnosis and appropriate treatment.
The management of a heart attack and heart block differs due to their distinct underlying causes and immediate risks. Here’s an overview of the management approaches for each condition:
Management of a Heart Attack (Myocardial Infarction):
- Immediate medical attention: A heart attack is a medical emergency, and it is crucial to call for emergency medical assistance (such as an ambulance) as soon as possible.
- Emergency medical care: Upon arrival at the hospital, the medical team will quickly assess the situation and provide immediate treatment, which may include:
- Oxygen therapy: Supplemental oxygen is administered to ensure adequate oxygen supply to the body.
- Medications: Aspirin or other antiplatelet medications may be given to help prevent further blood clotting. Nitroglycerin and/or pain medications may be provided to relieve chest pain or discomfort.
- Reperfusion therapy: Time-sensitive procedures such as percutaneous coronary intervention (PCI) or thrombolytic therapy may be performed to restore blood flow to the blocked coronary artery and minimize damage to the heart muscle.
- Post-acute care and management: After initial treatment, the patient will typically be admitted to the hospital for further monitoring and management, which may include:
- Medications: Medications such as antiplatelet agents, beta-blockers, ACE inhibitors, statins, and other appropriate drugs are prescribed to manage risk factors, improve heart function, prevent future complications, and aid in recovery.
- Cardiac rehabilitation: A structured program that combines exercise, education, counseling, and support to help patients recover, improve cardiovascular fitness, and reduce the risk of future heart problems.
- Lifestyle modifications: Emphasizing the importance of a heart-healthy diet, regular physical activity, smoking cessation, stress management, and maintaining a healthy weight.
- Follow-up care: Regular follow-up visits with a healthcare provider to monitor progress, assess the effectiveness of treatment, and adjust medications if needed.
Management of Heart Block (Atrioventricular Block):
- Evaluation and diagnosis: A healthcare provider will conduct a thorough evaluation to determine the underlying cause and severity of the heart block. This may involve a medical history review, physical examination, electrocardiogram (ECG), and other tests such as Holter monitoring or electrophysiological studies.
- Observation and monitoring: Depending on the severity of the heart block and associated symptoms, the healthcare provider may recommend monitoring the condition to assess any changes or progression.
- Medications: In some cases, causative medications such as beta-blockers or calcium channel blockers or other antiarrhythmic drugs should be stopped or medications such as Orciprenaline, Isoprenaline or Atropine my be given to manage symptoms, regulate heart rate, or improve the electrical conduction.
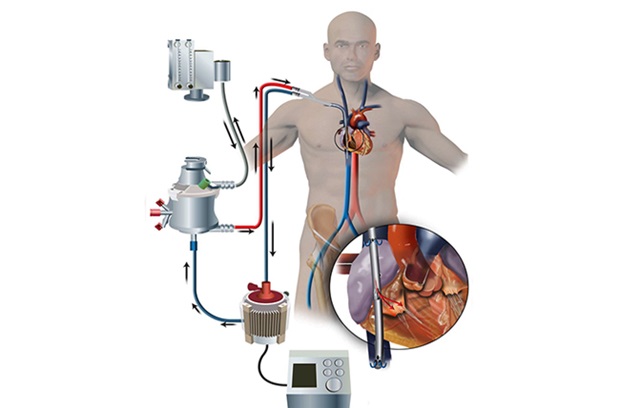
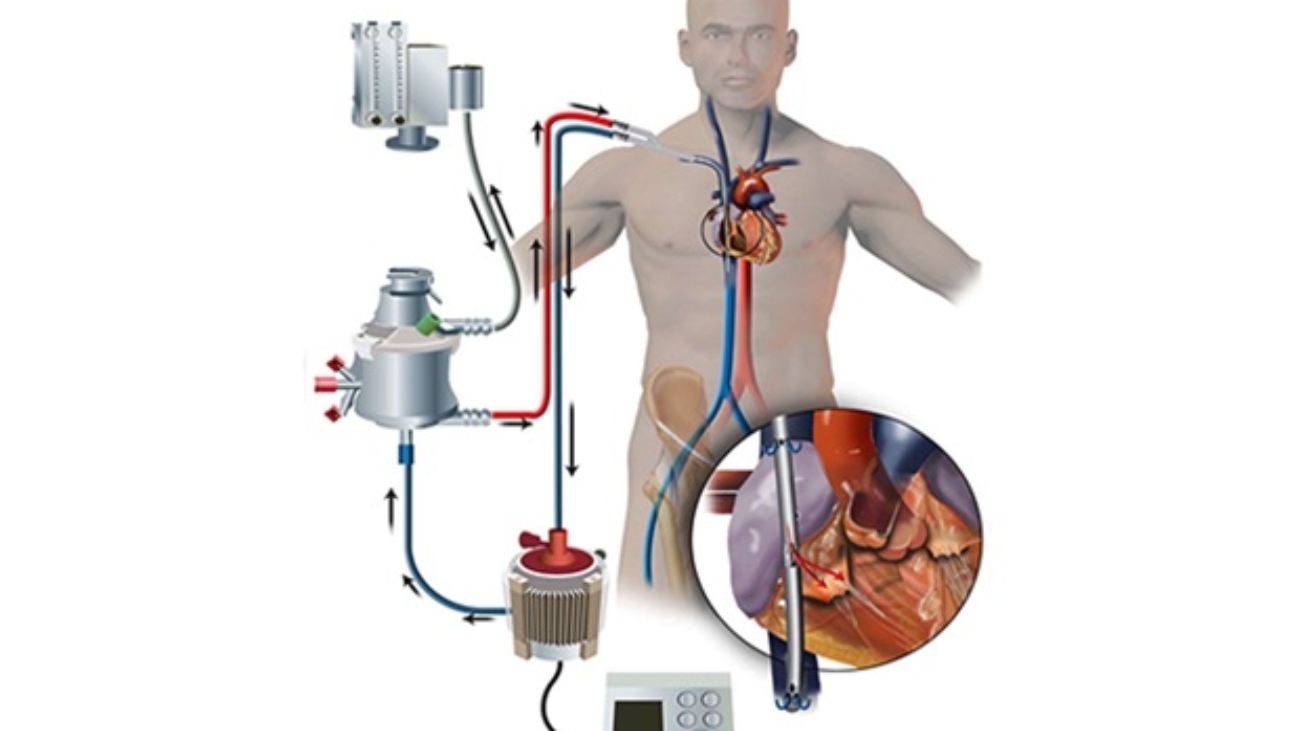
- Pacemaker: For more severe cases of heart block, a pacemaker may be implanted. It may be temporary or permanent. Temporary pacemaker is placed from groin to support heart rate temporarily till permanent pacemaker implanted. A pacemaker is a small device that helps regulate the heart’s electrical impulses and ensures a consistent and appropriate heart rate.
- Lifestyle modifications: Similar to heart attack management, lifestyle modifications play a crucial role in overall heart health. This includes adopting a heart-healthy diet, engaging in regular physical activity (as advised by healthcare providers), quitting smoking, managing stress, and maintaining a healthy weight.
It’s important to note that the management approach for both conditions may involve personalized and individualized care based on the specific needs, underlying conditions, and severity of the condition. Therefore, it is essential to consult with healthcare professionals for a thorough evaluation, accurate diagnosis, and tailored management plan.